Multiple Sclerosis vs Lyme Disease
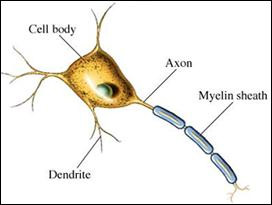
Multiple Sclerosis (MS) was first described by Jean-Martin Charcot in 1868, and is an autoimmune inflammatory disease in which the myelin sheath (composed of fats) around nerve axons of the brain and spinal cord are damaged. Chronic inflammation leads to widespread demyelination, especially in the white matter areas of the brain where there is a high density of fatty acids. MS affects the ability of nerve cells to communicate with each other because the body’s immune system attacks and damages the myelin sheath. As a result, lesions or scars in the brain and spinal cord give rise to neurological symptoms such as numbness and tingling.
MS onset usually occurs in young adults and is more common in women. Its estimated prevalence ranges between 2 and 150 per 100,000 people. The neurological symptoms associated with Multiple Sclerosis can vary, with new symptoms occurring either in discrete attacks (relapsing forms) or gradually accumulating over time (progressive form). Generally, the symptoms associated with MS include: changes in sensation, loss of sensitivity, prickling or numbness especially in the extremities, muscle weakness, clonus, muscle spasms, poor coordination, difficulty swallowing, visual problems, extreme fatigue, acute and chronic pain, and irritable bladder and bowel.
The pathophysiology of MS is not entirely known, however, we do know that there is a breakdown in the blood brain barrier (BBB), a capillary system that prevents immune cells and particularly T cells from entering the nervous system. The BBB is not normally permeable to these cells, but in MS it is and the T cells attack nervous system tissue. These T cells then recognize brain tissue as foreign and attack, which accounts for the autoimmune component of MS. Inflammation ensues causing further damage to fragile neural tissue.
Interestingly, the Pacific Northwest has one of the highest populations of MS patients in the United States, and no one seems to know exactly why this phenomenon exists. Theories as to why there appears to be a geographical association to MS prevalence has been suggested, such as decreased vitamin D levels due to lack of sunlight, genetic propensity, and/or infectious agents, but no definitive cause has been recognized.
Alan MacDonald, MD, a pathologist in Long Island, New York suggested that we rule out Lyme Disease as a causal agent of Multiple Sclerosis. In a scientific study authored by Alban, P, Johnson, P, and Nelson, D, in the Journal of Microbiology (2000), it was demonstrated in the laboratory that spirochetes are unable to manufacture their own fatty acids and therefore gravitate to places of high density fatty acids exhibiting “neurotropic behavior”. This would make sense in light of the fact that, Neuroborreliosis (neurological Lyme Disease) is often characterized by white matter lesions in the brain resembling those found in MS patients. Additionally, MS and Lyme Disease can both be relapsing diseases. I am not suggesting that ALL MS patients have Lyme Disease, but rather, that Lyme Disease should be considered in the differential diagnosis. White matter lesions on an MRI look the same whether the etiology is MS or Lyme Disease. However, lesions due to MS do not recede with antibiotic use, whereas lesions due to the bacteria that cause Lyme Disease may simply decrease in size or disappear with antibiotics.
To date there is no known cure for MS, and treatments including interferon may help to halt progression of the disease. However, if an underlying tick-borne infection is present, antibiotics that cross the blood brain barrier can be used. Follow up MRI tests can reveal that if infection is present, a receding of the white matter lesions occurs, and healing can take place. Return of total function may or may not occur depending on many factors including: genetic propensity, environmental influences, diet, length of time of infection, status of the immune system, and virulence of the strain of spirochete(s) present.
Western Blot IgM and IgG testing for Lyme Disease should be considered in patients with a diagnosis of Multiple Sclerosis who have known previous tick bites or who live in endemic areas where the exposure rate to ticks is high.
A diet low in fats known as the “Swank Diet” has been reported to aid in slowing the progression of MS symptoms. This makes sense in light of the fact that if the disease in question is caused by the spirochetal bacteria, providing fatty acid nutrients which these bacteria require to live and replicate, may decrease symptoms and neural inflammation by keeping the bacteria well fed and “happy”.