Lyme and Osteoporosis
Patients who have had or currently have Lyme Disease often experience an increased likelihood of developing osteopenia and/or osteoporosis (conditions of progressive bone loss, particularly in women). This may, at least in part, be due to the fact that calcium is sequestered from the bone by pathogenic organisms in order to anchor and stabilize their lattice structure biofilm in tissues and the vascular system. Presence in the urine of higher than normal amounts of PYD (Pyridinoline) and DPD (Deoxypyridinoline) indicates a rapid rate of bone loss. Biofilms may also contribute to calcium plaque formation in the vasculature and set the stage, at least in part, for the development of athersclerosis, particularly in the carotid arteries which impairs blood flow to the brain (personal communication Dr. Stephen Fry.)
Calcium concentrations in the bone and blood are tightly controlled by the parathyroid gland, which releases parathyroid hormone (PTH). PTH is secreted by the chief cells in the parathyroid gland, and serves to increase the concentration of calcium in the blood. Calcitonin, a hormone produced by the parafollicular cells of the thyroid gland, acts in opposition to PTH by decreasing calcium in the blood, and hence, a balance of both is required to maintain proper bone health. This balance often becomes compromised in conditions of chronic inflammation.
PTH and calcitonin regulate bone metabolism along with Vitamin D, calcium, phosphorus, and magnesium, and bone health can become compromised when any of these substances are out of balance. Simply living in the northern hemisphere predisposes one to be vitamin D deficient which is not insignificant given that Vitamin D also plays an important role in immune regulation. Generally I find that all of my patients need Vitamin D supplementation.
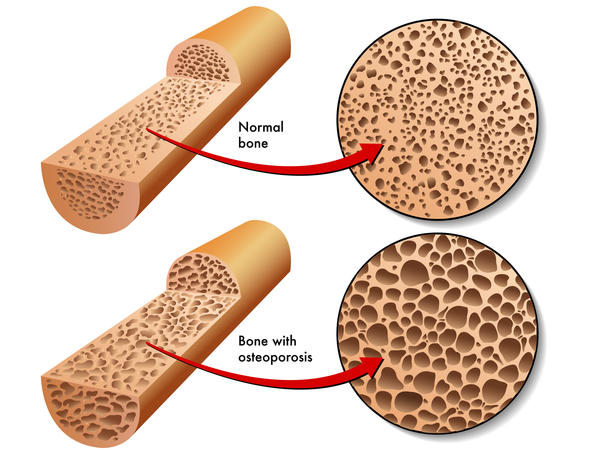
When infection and chronic inflammation affect the parathyroid gland, the gland activates cells known as osteoblasts (bone building), which then transform into osteoclasts (bone breaking down), which dissolve mineralized collagen in bone, causing osteopenia and/or osteoporosis.
Measurements of bone resorption (DEXA scan), and urine N- terminal telopeptide and C terminal telopeptide can help identify where a patient is on the continuum of normal bone resorption to osteoporosis. Nutritional interventions can then be initiated early on in order to avoid the onset of more severe bone degenerative disease. Dr. Marra can help you identify whether or not this is a potential problem for you and help you correct the problem naturally.